Chronic Obstructive Pulmonary Disease (COPD)
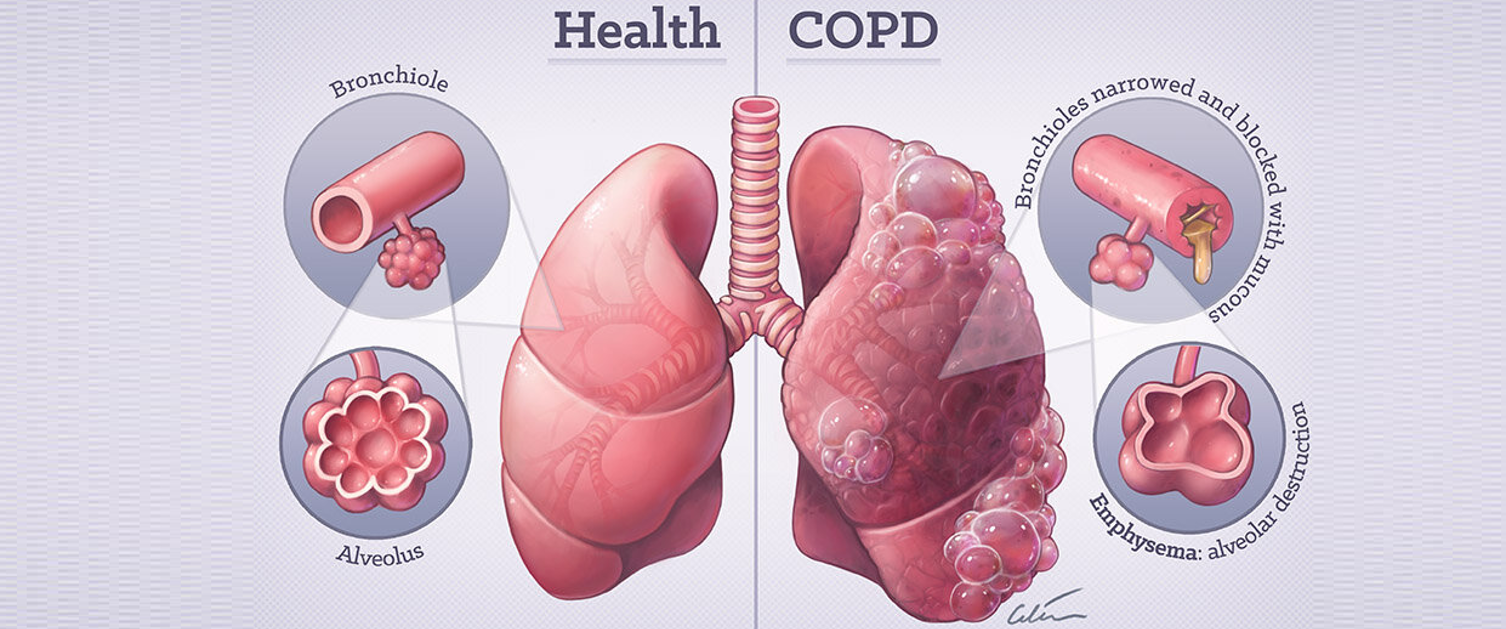
COPD describes a group of lung function conditions that make it difficult to empty air out of the lungs because your airways have been narrowed.
Two of the lung conditions are:
- Bronchitis – this means the airways are inflamed and narrowed, often producing sputum or phlegm.
- Emphysema – this is when the air sacs at the end of the airways break down making lungs baggy and full of holes which trap air.
These narrow the airways which makes it harder to move air in and out. This means your lungs are less able to take in oxygen and get rid of carbon dioxide. There are treatments to help you breathe more easily, but they cannot reverse the damage to your lungs.
What causes COPD?
COPD usually develops because of long term damage to your lungs from breathing in a harmful substance. This is usually cigarette smoke, however smoke from other sources, air pollution, dust, fumes, and chemicals can also contribute to developing COPD.
You are more likely to develop COPD if you are 35 and over and are either a current or ex-smoker.
COPD can also run in families, so if your parents had chest problems then your own risk is higher.
What are the symptoms?
- Getting short of breath easily when you do everyday things.
- Having a cough that lasts a long time.
- Wheezing in cold weather
- Producing more sputum than usual.
These symptoms may be present all the time, or they may appear to get worse when you have a n infection or breathe in smoke fumes.
People with severe COPD can also experience loss of weight, loss of appetite and swelling in the ankles.
How is COPD diagnosed?
Your GP will ask about your breathing, how your daily life is affected and your general health. You will be asked if you’ve smoked or have been exposed to duct, fumes and chemicals.
We can check how well your lungs are working with a Spirometry test. This involves blowing hard into a machine which measures your lung capacity and how quickly you empty your lungs. They may also check your oxygen levels, how often your symptoms flare up and how short of breath you feel during everyday activities.
Your doctor should also arrange a blood test and chest x-ray to rule out other causes of your symptoms.
Your body mass index (BMI) will also be calculated to find out if you are a healthy weight. This is important because you can deal with COPD better if you’re not overweight or underweight.
You may also be seen by other health care professionals, such as physiotherapists, dieticians and occupational therapists who can also help you manage your condition and make daily life easier.
I treatment plan will be agreed with your doctor or nurse, and it is recommended you have a regular check up at least once a year.
Medications
There are several types of medicine to improve symptoms like breathlessness and to help prevent a flare up.
- Bronchodilators – A type of medicine you inhale to open up your airways and help you breathe more easily.
- Steroid Inhaler – If you experience regular flare ups, you may be given one of these to help reduce inflammation and swelling in your airways.
- Mucolytic – This can be prescribed if you cough up a lot of sputum to make it thinner and easier to cough up.
- Oxygen
If you have low level oxygen in your blood, your health care team may send you to a specialist to see if oxygen can help you. If oxygen levels drop when you’re active you might be given Ambulatory Oxygen, which is a small portable cylinder. If your oxygen levels are low when you’re resting, you may be offered long-term oxygen therapy in your home.
Managing your COPD
- Don’t smoke.
- Eat well and stay a healthy weight.
- Keep active and exercise.
- Control your breathing.
Managing Flare ups
A flare up also referred to as an exacerbation is when your symptoms become particularly severe. You should have an action plan that you’ve agreed with your health care professional, so you know what to do. Your plan may include a rescue pack of drugs which normally consist of steroids and antibiotics which you keep at home.
Take care of your feelings
Living with a long-term condition is not easy. The physical symptoms such as breathlessness and coughing can mean you feel stressed, anxious or depressed.
It is important to remember not to bottle things up, talking to a friend, relative or healthcare professional can help, stay active and sociable, and learn more about COPD as this will help you to understand and cope better with your condition.