Women's Health

Pelvic floor dysfunction is common amongst women and can lead to a variety of symptoms. Examples of pelvic floor dysfunction include:
- Urinary frequency and urgency (needing to pass urine more often and rushing to pass urine)
- Urinary incontinence (bladder leaks)
- Pelvic organ prolapse
- Bowel incontinence (bowel leakage)
You can find out more in this leaflet: Lets talk about continence
Below is further information and resources to help you find ways of managing some of your symptoms. If you are still experiencing symptoms and would like further assessment from a pelvic health physiotherapist, please complete the self-referral link below
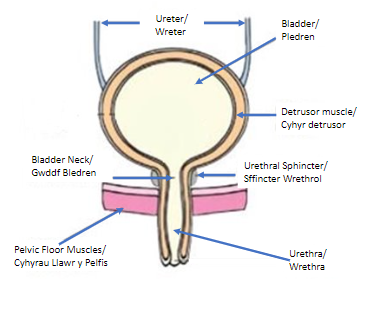
The kidneys filter our blood to remove excess water, waste, and produce urine, which travels along the ureters to the bladder. The bladder stores the urine and then empties it out.
We tend to get the initial desire to pass urine when it is holding approximately 150mls, but we often ignore these first signs. Generally, people visit the toilet to pass urine when it is convenient, and the bladder is holding approximately 400mls urine. This volume tends to be larger for the first void (wee) of the day.
A healthy bladder will need emptying up to 6-8 times per day, and not more than once during the night.
A healthy bladder should give us plenty of warning when it is getting full, be free of infections, and empty fully without pain or blood in our urine.
Aim to drink between 1.5 – 2 litres (6-8 mugs) daily.
Urinary incontinence is a common condition affecting 1 in 3 women. However, it should not be accepted as the norm and can improve with simple advice and exercises found below:
There are two main types of urinary incontinence:
Stress and urge incontinence can also occur together and this is known as mixed incontinence.
Bladder Frequency, urgency and urge incontinence may be due to an overactive bladder
If you are experiencing stress incontinence and/or urge incontinence strengthening your pelvic floor muscles can help to improve your symptoms – see the Pelvic floor exercises section for more information on this.
Healthy bladder habits
You may want to avoid drinks that can irritate the bladder if you experience urinary frequency, urgency or urge incontinence.
Bladder training
Bladder training can often help to reduce frequency, urgency and urge incontinence. This is explained in this leaflet - Bladder Training
Here is an example of a bladder diary (as described in the leaflet) that you can complete - Bladder Diary
If you have difficulty fully emptying your bladder, see the link below for helpful techniques
Pelvic floor dysfunction
Pelvic floor dysfunction can contribute to difficulties emptying the bladder. This can be due to either a weak or a tense pelvic floor. Assessment by a pelvic health physiotherapist will be able to guide you on whether your pelvic floor muscle needs strengthening or releasing if the above hasn't worked.
You may have been referred for investigations by your Consultant, Urology Nurse or Bladder and Bowel Nurse. The links below provide information regarding two common bladder tests:
Healthy bowel
Healthy bowel habits are important as straining to empty your bowels can make urinary incontinence worse, see the healthy bowel section for more advice.
Menopausal symptoms
Menopausal symptoms can influence pelvic floor dysfunction symptoms. See the menopause section for some useful information regarding the menopause.
Healthy Bowels should empty anything between 3 times per day and 3 times per week.
A stool should be easily passed without straining, pain, or blood.
It is important to avoid constipation and straining to empty your bowels as this can contribute to pelvic floor dysfunction.

Adjusting your position on the toilet

Drinking enough fluids

Eating plenty of fibre
All of the above can help, along with taking any medication prescribed for you. If you have difficulty emptying your bowels the section below has more information on this.
Constipation refers to infrequency or difficulty opening your bowels, where stools may be hard, lumpy or painful to pass.
Further information and tips for avoiding constipation can be found below:
- Constipation (NHS)
- Constipation (Guts UK)
- Fibre Fact Sheet (BDA)
- Tips to Encourage Healthy Bowel Habits
- Improving your Bowel Function - POGP
It is important that you regularly check your stools to rule out more serious conditions that can affect bowel function.
Key signs and symptoms to look out for can be found on the bowel cancer UK website - Bowel Cancer Symptoms
Adapting the position you use to sit on the toilet can help ‘straighten out’ the back passage, which makes it easier to pass stools. This sheet gives information about the best position to use - Correct Position for Emptying Bowels
The following videos may also be useful:
- How To Open Your Bowels Without Straining (Michelle Kenway)
- 'I Love You' Abdominal Massage (ECO Physiotherapy)
It is also important to ensure you fully relax the pelvic floor when passing a stool, difficulty relaxing the pelvic floor can also contribute to problems with emptying.
The video below guides you through techniques to encourage relaxation of the pelvic floor whilst on the toilet:
Pelvic floor dysfunction can contribute to difficulties emptying the bowels. This can be due to either a weak or a tense pelvic floor. Assessment by a pelvic health physiotherapist will be able to guide you on whether your pelvic floor muscle needs strengthening or releasing if the above hasn't worked.
Menopausal symptoms can influence pelvic floor dysfunction symptoms. See the menopause section for some useful information regarding the menopause.
Bowel control problems can affect people in different ways:
- Sudden urges to poo that you can’t control
- Accidental bowel leakage
- Being unable to hold on to wind
The information below may be helpful:
Your pelvic floor muscles are responsible for controlling both your bladder and your bowels. Improving your pelvic floor strength can help to manage these symptoms. See the pelvic floor exercise section for further information on this.
Menopausal symptoms can influence pelvic floor dysfunction symptoms. See the menopause section for some useful information regarding the menopause.
The Pelvic Floor Muscles are a group of muscles that span the underside of your pelvis, forming the ‘floor’ of your pelvis. They insert into the pubic bone at the front, they fan out to the side into your sitting bones, and then into your tailbone/coccyx at the back.
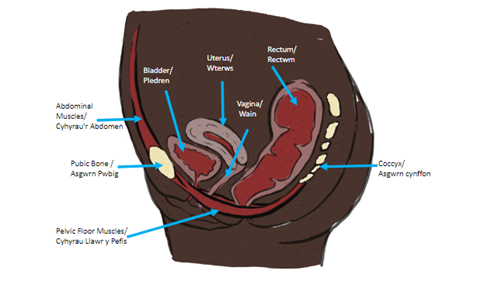
The Pelvic Floor Muscles support the bladder, reproductive organs, and bowels inside the pelvis, keep us continent of urine and faeces, provides stability to the spine and pelvis when we are active, and have an important role in sexual function.
During pregnancy, the pelvic floor muscles and ligaments can become stretched, lengthened and weakened as they cope with increased load as your baby grows, hormonal changes, and labour.
Doing Pelvic Floor Muscle Exercises during pregnancy is therefore important to help with bladder and bowel leakage, developing prolapse symptoms, and to reduce the likelihood of developing Pelvic Girdle Pain - See further information on this in the relevant section below.
How to find and exercise your pelvic floor muscles:
- Lie down or sit upright, in a comfortable position.
- Imagine that you are stopping yourself from passing wind and then stopping the flow of urine
- It should feel like a squeeze and lift up of the pelvic floor muscles from the back passage towards the bladder
- Other cues that can help engage your pelvic floor muscle include:
- Squeezing your pubic bone and your tail bone together
- Pretending you have a tail and curling it between your legs
- Imagine you are sucking up a marble with your back passage
- Continue to breath normally, don’t hold your breath or squeeze your buttocks or leg muscles, and ensure you fully relax after every squeeze
How often should we do them?
- Long squeezes - tighten up your pelvic floor muscles, hold the squeeze, then release/relax them fully. How long can you hold it for?
Repeat the long squeezes until the muscles fatigue. How many times can you repeat it?
Aim eventually to do 10 second holds and repeat 10 times
- Short Squeezes – quickly tighten up your pelvic floor muscles, then immediately release/relax them fully. How many times can you do this before the muscles fatigue?
Aim eventually to do these 10 times
- Repeat these exercises 3 times each day and try to do them in lie, sit or stand. Sitting or lying down will be easier to start with
- It is important to fully release/relax in between each squeeze. The aim is to have strong muscles that can fully lengthen too. ‘Pulsing’ your muscles could shorten them.
Further information and resources on Pelvic Floor Muscles can be found below:
This animation shows the location of your pelvic floor muscles – Pelvic Floor Anatomy
The following is a video and leaflet explaining pelvic floor muscle exercises further:
Squeezy: pelvic floor support app (squeezyapp.com)
The POGP (Pelvic, Obstetric and Gynaecological Physiotherapy), a UK based Physiotherapy Professional Network affiliated to the Chartered Society of Physiotherapy have put together this leaflet explaining Pelvic Organ Prolapse and how to reduce the symptoms that you can read through here
Some women find it helps to support the perineum (the area between the vagina and back passage) with a clean pad or toilet paper.
Strengthening weak pelvic floor muscles can help to prevent or reduce pelvic organ prolapse symptoms. They can be strengthened by doing regular pelvic floor muscle exercises. See the pelvic floor exercise section for further information on this.
The POGP (Pelvic, Obstetric and Gynaecological Physiotherapy website contains useful information about using a pessary to manage prolapse symptoms.
Healthy bowel habits are important as straining to empty your bowels can make prolapse symptoms worse, see the healthy bowel section for more advice
Menopausal symptoms can influence pelvic floor dysfunction symptoms. See the menopause section for some useful information regarding the menopause
 Pain during and/or after sex is known as dyspareunia - Dyspareunia – Pain with Intercourse
Pain during and/or after sex is known as dyspareunia - Dyspareunia – Pain with Intercourse
There are many causes of dyspareunia. Some women have tension in their pelvic floor muscles (sometimes known as an overactive or tight pelvic floor) and this may contribute to pain having sex. If you think you may have tension in your pelvic floor and would like to check, please see this information slide here
See below for some useful information that you may find helpful if you have an overactive or tight pelvic floor:
- Pelvic Floor Muscle Release Techniques
- Diaphragmatic Breathing
- Guided Visualization for Elimination (Constipation, Urinary Hesitancy, Incomplete Bladder Emptying)
- Pelvic Floor Release Stretches | FemFusion Fitness
- 3 Visualisations for Pelvic Floor Relaxation
- Guided Meditation for Pelvic Floor Relaxation
- Top 3 Pelvic Floor Stretches for Women and Men
- Easy Stretches to Relax the Pelvis
Vaginal dryness can be a cause of pain during intercourse. If you haven’t already, trying a natural lubricant can sometimes reduce this discomfort. There are a number of different types of lubricant including water based, oil based and silicone based. If you have tried these and are still having pain with intercourse, this is something Physiotherapy may be able to support you with.
Taking care of the vulval (genital area) skin is important - Care of Vulval Skin
This leaflet is useful if you have found having a smear test painful - Smears Without Tears
 We see many women who have been referred to physiotherapy due to symptoms of persistent (also known as chronic) pelvic pain. These can include bladder pain syndrome (interstitial cystitis), chronic pelvic pain and vulvodynia:
We see many women who have been referred to physiotherapy due to symptoms of persistent (also known as chronic) pelvic pain. These can include bladder pain syndrome (interstitial cystitis), chronic pelvic pain and vulvodynia:
See below for some useful information that you may find helpful if you have a persistent pain condition:
The ‘Education Programmes for Patients’ offer self-management health and wellbeing 6 week courses, including one focused on chronic pain. Participants need to self-refer (the form is on website below). The website also has some video relaxation sessions, and other resources.
See below for some useful information that you may find helpful if you have an overactive or tight pelvic floor:
- Pelvic Floor Muscle Release Techniques
- Diaphragmatic breathing
- Guided Visualization for Elimination (Constipation, Urinary Hesitancy, Incomplete Bladder Emptying)
- Pelvic Floor Release Stretches | FemFusion Fitness
- 3 Visualisations for Pelvic Floor Relaxation
- Guided Meditation for Pelvic Floor Relaxation
- Top 3 Pelvic Floor Stretches for Women and Men
- Easy Stretches to Relax the Pelvis
Taking care of the vulval (genital area) skin is important - Care of Vulval Skin
This leaflet is useful if you have found having a smear test painful Smears without Tears
If you have endometriosis Endo Cymru has some useful information and you can also contact Endometriosis UK for support.
The Vulval Pain Society provides support for women with vulval pain.
Menopausal symptoms can influence pelvic floor dysfunction symptoms. See below for some useful information regarding the menopause:
 OAK Menopause
OAK Menopause
There are education sessions run to better understand the menopause. You must be registered with a GP within Gwent to access these sessions.
If you would like to register your interest or find out more about the upcoming sessions
Contact methods
- OAK Menopause : 01495 768645
- OAKReferrals.ABB@wales.nhs.uk
Information and fact sheets about menopause are available from:
- Womens Health Concern
- Rock My Menopause
- Menopause Matters
- Menopause
- Diet During the Menopause - Association of UK Dietetics
- Menopause Matters UK
- Vaginal Dryness
- HRT
- Alternatives to HRT
Information for women diagnosed with premature ovarian insufficiency:
Aneurin Bevan University Health Board and partners have developed the ‘melo’ website to look after the mental wellbeing of its residents. Melo can help you to develop new skills that will support you when life is difficult.

Melo Cymru - Mental Wellbeing Resources, Courses + Advice Gwent Wales
Maintaining a healthy weight can help to alleviate bladder leakage symptoms
Weight Management Service - Aneurin Bevan University Health Board (nhs.wales)

Stopping Smoking can help to alleviate bladder leakage by reducing coughing associated with smoking - Help Me Quit
Exercise

Domestic abuse is not acceptable; anyone experiencing domestic violence and abuse is not to blame and is not alone. Help and support is available.
